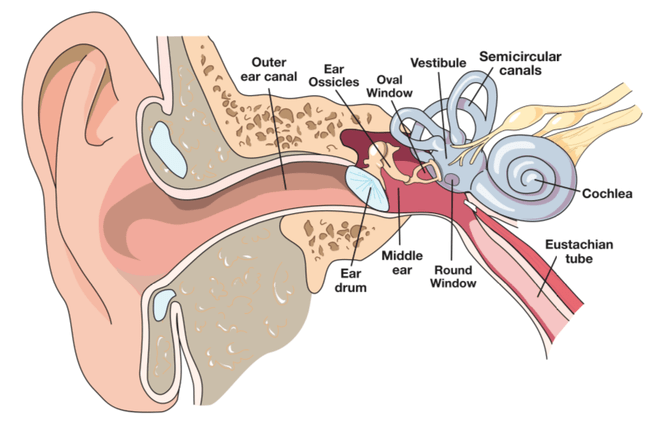
Human ear anatomy
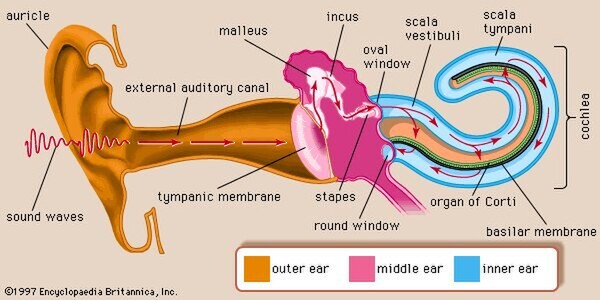
The human ear, like that of other mammals, contains sense organs that serve two quite different functions: that of hearing and that of postural equilibrium and coordination of head and eye movements. Anatomically, the ear has three distinguishable parts: the outer, middle, and inner ear.
The outer ear consists of the visible portion called the auricle, or pinna, which projects from the side of the head, and the short external auditory canal, the inner end of which is closed by the tympanic membrane, commonly called the eardrum. The function of the outer ear is to collect sound waves and guide them to the tympanic membrane. The middle ear is a narrow air-filled cavity in the temporal bone. It is spanned by a chain of three tiny bones - the malleus (hammer), incus (anvil), and stapes (stirrup), collectively called the auditory ossicles. This ossicular chain conducts sound from the tympanic membrane to the inner ear. It is a complicated system of fluid-filled passages and cavities located deep within the rock-hard petrous portion of the temporal bone. The inner ear consists of two functional units: the vestibular apparatus, consisting of the vestibule and semicircular canals, which contains the sensory organs of postural equilibrium; and the snail-shell-like cochlea, which contains the sensory organ of hearing. These sensory organs are highly specialized endings of the eighth cranial nerve, also called the vestibulocochlear nerve.
Outer ear
The most-striking differences between the human ear and the ears of other mammals are in the structure of the outermost part, the auricle. In humans the auricle is an almost rudimentory, usually immobile shell that lies close to the side of the head. It consists of a thin plate of yellow elastic cartilage covered by closely adherent skin.
The cartilage is moulded into clearly defined hollows, ridges, and furrows that form an irregular shallow funnel. The deepest depression, which leads directly to the external auditory canal, or acoustic meatus, is called the concha. It is partly covered by two small projections, the tonguelike trigs in front and the antitragus behind. Above the tragus a prominent ridge, the helix, arises from the floor of the concha and continues as the incurved rim of the upper portion of the auricle. An inner, concentric ridge, the antihelix, surrounds the concha and is separated from the helix by a furrow, the scapha, also called the fossa of the helix. In some ears a little prominence known as Darwin’s tubercle is seen along the upper, posterior portion of the helix; it is the vestige of the folded-over point of the ear of a remote human ancestor.
The lobule, the fleshy lower part of the auricle, is the only area of the outer ear that contains no cartilage. The auricle also has several small rudimentary muscles, which fasten it to the skull and scalp. In most individuals these muscles do not function, although some persons can voluntarily activate them to produce limited movements. The external auditory canal is a slightly curved tube that extends inward from the floor of the concha and ends blindly at the tympanic membrane. In its outer third, the wall of the canal consists of cartilage; in its inner two-thirds, of bone. The entire length of the passage (24 mm, or almost 1 inch) is lined with skin, which also covers the outer surface of the tympanic membrane. Fine hairs directed outward and modified sweat glands that produce earwax, or cerumen, line the canal and discourage insects from entering it.
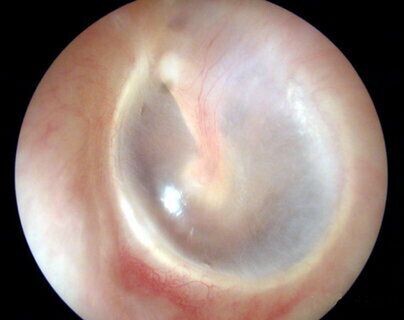
Tympanic membrane (Ear drum)
The thin semitransparent tympanic membrane, or eardrum, which forms the boundary between the outer ear and the middle ear, is stretched obliquely across the end of the external canal. Its diameter is about 8–10 mm (about 0.3–0.4 inch), it's shape that of a flattened cone with its apex directed inward. Thus, its outer surface is slightly concave. The edge of the membrane is thickened and attached to a groove in an incomplete ring of bone, the tympanic annulus, which almost encircles it and holds it in place. The uppermost small area of the membrane where the ring is open, the pars flaccida, is slack, but the far greater portion, the pars tensa, is tightly stretched. The appearance and mobility of the tympanic membrane are important for the diagnosis of middle-ear disease, which is especially common in young children. When viewed with the otoscope, the healthy membrane is translucent and pearl-gray in colour, sometimes with a pinkish or yellowish tinge.
The entire tympanic membrane consists of three layers. The outer layer of skin is continuous with that of the external canal. The inner layer of mucous membrane is continuous with the lining of the tympanic cavity of the middle ear. Between these layers is a layer of fibrous tissue made up of circular and radial fibres that give the membrane its stiffness and tension. The membrane is well supplied with blood vessels and sensory nerve fibres that make it acutely sensitive to pain.
Middle-ear cavity
The cavity of the middle ear is a narrow air-filled space. A slight constriction divides it into an upper and a lower chamber, the tympanum (tympanic cavity) proper below and the epitympanum above. These chambers are also referred to as the atrium and the attic, respectively. The middle-ear space roughly resembles a rectangular room with four walls, a floor, and a ceiling. The outer (lateral) wall of the middle-ear space is formed by the tympanic membrane. The ceiling (superior wall) is a thin plate of bone that separates the middle-ear cavity from the cranial cavity and brain above. The floor (inferior wall) is also a thin bony plate, in this case separating the middle-ear cavity from the jugular vein and the carotid artery below.
The back (posterior) wall partly separates the middle-ear cavity from another cavity, the mastoid antrum, but an opening in this wall leads to the antrum and to the small air cells of the mastoid process, which is the roughened, slightly bulging portion of the temporal bone just behind the external auditory canal and the auricle. In the front (anterior) wall is the opening of the eustachian tube (or auditory tube), which connects the middle ear with the nasopharynx.
The inner (medial) wall, which separates the middle ear from the inner ear, or labyrinth, is a part of the bony otic capsule of the inner ear. It has two small openings, or fenestrae, one above the other. The upper one is the oval window, which is closed by the footplate of the stapes. The lower one is the round window, which is covered by a thin membrane.
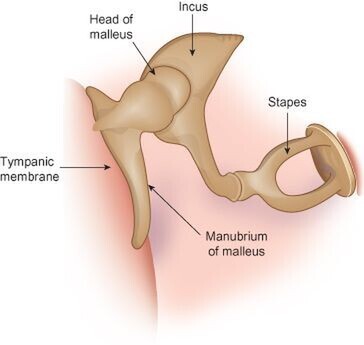
Auditory ossicles
Crossing the middle-ear cavity is the short ossicular chain formed by three tiny bones that link the tympanic membrane with the oval window and inner ear. From the outside inward they are the malleus (hammer), the incus (anvil), and the stapes (stirrup). The malleus more closely resembles a club than a hammer, and the incus looks more like a premolar tooth with uneven roots than an anvil. These bones are suspended by ligaments, which leave the chain free to vibrate in transmitting sound from the tympanic membrane to the inner ear.
The malleus consists of a handle and a head. The handle is firmly attached to the tympanic membrane from the centre (umbo) to the upper margin. The head of the malleus and the body of the incus are joined tightly and are suspended in the epitympanum just above the upper rim of the tympanic annulus, where three small ligaments anchor the head of the malleus to the walls and roof of the epitympanum.
Another minute ligament fixes the short process (crus) of the incus in a shallow depression, called the fossa incudis, in the rear wall of the cavity. The long process of the incus is bent near its end and bears a small bony knob that forms a loose ligament-enclosed joint with the head of the stapes. The stapes is the smallest bone in the body. It is about 3 mm (0.1 inch) long and weighs scarcely 3 mg (0.0001 ounce). It lies almost horizontally, at right angles to the process of the incus. Its base, or footplate, fits nicely in the oval window and is surrounded by the elastic annular ligament, although it remains free to vibrate in transmitting sound to the labyrinth.
Muscles
Two minuscule muscles are located in the middle ear. The longer muscle, called the tensor tympani, emerges from a bony canal just above the opening of the eustachian tube and runs backward and then outward as it changes direction in passing over a pulleylike projection of bone. The tendon of this muscle is attached to the upper part of the handle of the malleus. When contracted, the tensor tympani tends to pull the malleus inward and thus maintains or increases the tension of the tympanic membrane.
The shorter, stouter muscle, called the stapedius, arises from the back wall of the middle-ear cavity and extends forward and attaches to the neck of the head of the stapes. Its reflex contractions tend to tip the stapes backward, as if to pull it out of the oval window. Thus, it selectively reduces the intensity of sounds entering the inner ear, especially those of lower frequency.
Nerves
The seventh cranial nerve, called the facial nerve, passes by a somewhat circuitous route through the facial canal in the petrous portion of the temporal bone on its way from the brainstem to the muscles of expression of the face. A small but important branch, the chorda tympani nerve, emerges from the canal into the middle-ear cavity and runs forward along the inner surface of the pars tensa of the membrane, passing between the handle of the malleus and the long process of the incus. Since at this point it is covered only by the tympanic mucous membrane, it appears to be quite bare. Then it resumes its course through the anterior bony wall, bringing sensory fibres for taste to the anterior two-thirds of the tongue and parasympathetic secretory fibres to salivary glands.
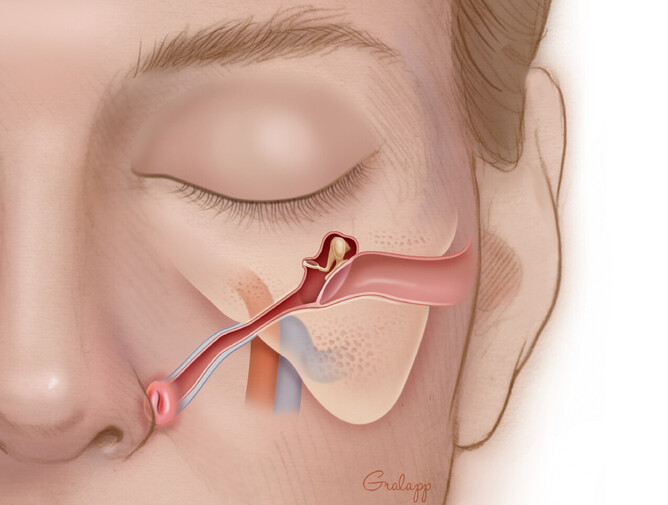
Eustachian tube
The eustachian tube, about 31–38 mm (1.2–1.5 inches) long, leads downward and inward from the tympanum to the nasopharynx, the space that is behind and continuous with the nasal passages and is above the soft palate. At its upper end the tube is narrow and surrounded by bone. Nearer the pharynx it widens and becomes cartilaginous. Its mucous lining, which is continuous with that of the middle ear, is covered with cilia, small hairlike projections whose coordinated rhythmical sweeping motions speed the drainage of mucous secretions from the tympanum to the pharynx.
The eustachian tube helps ventilate the middle ear and maintain equal air pressure on both sides of the tympanic membrane. The tube is closed at rest and opens during swallowing so that minor pressure differences are adjusted without conscious effort. During an underwater dive or a rapid descent in an airplane, the tube may remain tightly closed. The discomfort that is felt as the external pressure increases can usually be overcome by attempting a forced expiration with the mouth and nostrils held tightly shut. This maneuver, which raises the air pressure in the pharynx and causes the tube to open, is called the Valsalva maneuver, named for Italian physician-anatomist Antonio Maria Valsalva (1666–1723), who recommended it for clearing pus from an infected middle ear.
Inner ear
There are actually two labyrinths of the inner ear, one inside the other, the membranous labyrinth contained within the bony labyrinth. The bony labyrinth consists of a central chamber called the vestibule, the three semicircular canals, and the spirally coiled cochlea. Within each structure, and filling only a fraction of the available space, is a corresponding portion of the membranous labyrinth: the vestibule contains the utricle and saccule, each semicircular canal its semicircular duct, and the cochlea its cochlear duct. Surrounding the membranous labyrinth and filling the remaining space is the watery fluid called perilymph. It is derived from blood plasma and resembles but is not identical with the cerebrospinal fluid of the brain and the aqueous humour of the eye. Like most of the hollow organs, the membranous labyrinth is lined with epithelium (a sheet of specialized cells that covers internal and external body surfaces). It is filled with a fluid called endolymph, which has a markedly different ionic content from perilymph. Because the membranous labyrinth is a closed system, the endolymph and perilymph do not mix.
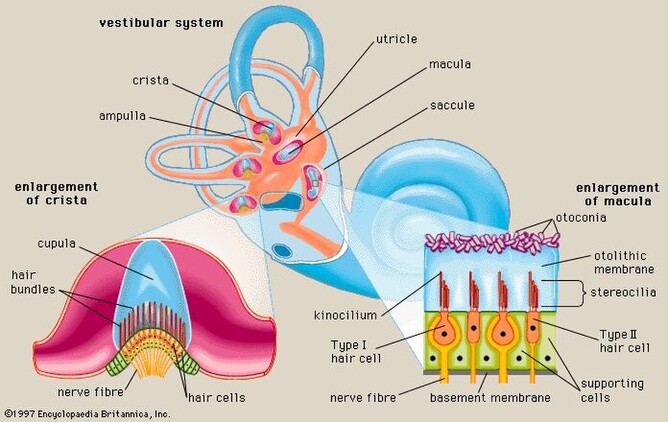
Vestibular system
The vestibular system is the apparatus of the inner ear involved in balance. It consists of two structures of the bony labyrinth, the vestibule and the semicircular canals, and the structures of the membranous labyrinth contained within them.
Vestibule
The two membranous sacs of the vestibule, the utricle and the saccule, are known as the otolith organs. Because they respond to gravitational forces, they are also called gravity receptors. Each sac has on its inner surface a single patch of sensory cells called a macula, which is about 2 mm (0.08 inch) in diameter. The macula monitors the position of the head relative to the vertical. In the utricle the macula projects from the anterior wall of that tubular sac and lies primarily in the horizontal plane. In the saccule the macula is in the vertical plane and directly overlies the bone of the inner wall of the vestibule. In shape it is elongated and resembles the letter J. Each macula consists of neuroepithelium, a layer that is made up of supporting cells and sensory cells, as well as a basement membrane, nerve fibres and nerve endings, and underlying connective tissue. The sensory cells are called hair cells because of the hairlike cilia—stiff nonmotile stereocilia and flexible motile kinocillia - that project from their apical ends. The nerve fibres are from the superior, or vestibular, division of the vestibulocochlear nerve. They pierce the basement membrane and, depending on the type of hair cell, either end on the basal end of the cell or form a calyx, or cuplike structure, that surrounds it.
Each of the hair cells of the vestibular organs is topped by a hair bundle, which consists of about 100 fine nonmotile stereocilia of graded lengths and a single motile kinocilium. The stereocilia are anchored in a dense cuticular plate at the cell’s apex. The single kinocilium, which is larger and longer than the stereocilia, rises from a noncuticular area of the cell membrane at one side of the cuticular plate. The longest stereocilia are those closest to the kinocilium; the stereocilia decrease in length in stepwise fashion away from the kinocilium.
Minute filamentous strands link the tips and shafts of neighbouring stereocilia to one another. When the hair bundles are deflected—e.g., because of a tilt of the head—the hair cells are stimulated to alter the rate of the nerve impulses that they are constantly sending via the vestibular nerve fibres to the brainstem. Covering the entire macula is a delicate acellular structure, the otolithic, or statolithic, membrane. This membrane is sometimes described as gelatinous, although it has a fibrillar pattern. The surface of the membrane is covered by a blanket of rhombohedral crystals, referred to as otoconia or statoconia, which consist of calcium carbonate in the form of calcite. These crystalline particles, which range in length from 1 to 20 μm (1 μm = 0.000039 inch), are much denser than the membrane—their specific gravity is almost three times that of the membrane and the endolymph—and thus add considerable mass to it.
The vestibular hair cells are of two types: type I cells have a rounded body enclosed by a nerve calyx, and type II cells have a cylindrical body with nerve endings at the base. They form a mosaic on the surface of the maculae, with the type I cells dominating in a curvilinear area (the striola) near the centre of the macula and the cylindrical cells around the periphery. The significance of these patterns is poorly understood, but they may increase sensitivity to slight tilting of the head.
Semicircular canals
The three semicircular canals of the bony labyrinth are designated according to their position: superior, horizontal, and posterior. The superior and posterior canals are in diagonal vertical planes that intersect at right angles. Each canal has an expanded end, the ampulla, which opens into the vestibule. The ampullae of the horizontal and superior canals lie close together, just above the oval window, but the ampulla of the posterior canal opens on the opposite side of the vestibule. The other ends of the superior and posterior canals join to form a common stem, or crus, which also opens into the vestibule. Nearby is the mouth of a canal called the vestibular aqueduct, which opens into the cranial cavity. The other end of the horizontal canal has a separate opening into the vestibule. Thus, the vestibule completes the circle for each of the semicircular canals.
Each of the three bony canals and its ampulla enclose a membranous semicircular duct of much smaller diameter that has its own ampulla. The membranous ducts and ampullae follow the same pattern as the canals and ampullae of the bony labyrinth, with their openings into the utricle and with a common crus for the superior and posterior ducts. Like the other parts of the membranous labyrinth, they are filled with endolymph and surrounded by perilymph. The narrow endolymphatic duct passes from the utricle through the vestibular aqueduct into the cranial cavity, carrying excess endolymph to be absorbed by the endolymphatic sac.
Each membranous ampulla contains a saddle-shaped ridge of tissue called the crista, the sensory end organ that extends across it from side to side. The crista is covered by neuroepithelium, with hair cells and supporting cells. From this ridge rises a gelatinous structure, the cupula, which extends to the roof of the ampulla immediately above it, dividing the interior of the ampulla into two approximately equal parts. Like the hair cells of the maculae, the hair cells of the cristae have hair bundles projecting from their apices. The kinocilium and the longest stereocilia extend far up into the substance of the cupula, occupying fine parallel channels. Thus, the cupula is attached at its base to the crista but is free to incline toward or away from the utricle in response to the slightest flow of endolymph or a change in pressure. The tufts of cilia move with the cupula and, depending on the direction of their bending, cause an increase or a decrease in the rate of nerve impulse discharges carried by the vestibular nerve fibres to the brainstem.
Cochlea
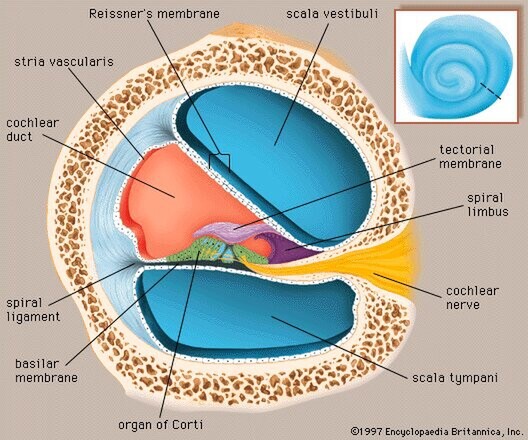
Structure of the cochlea
The cochlea contains the sensory organ of hearing. It bears a striking resemblance to the shell of a snail and in fact takes its name from the Greek word for this object. The cochlea is a spiral tube that is coiled two and one-half turns around a hollow central pillar, the modiolus. It forms a cone approximately 9 mm (0.35 inch) in diameter at its base and 5 mm in height. When stretched out, the spiral tube is approximately 30 mm in length. It is widest—2 mm—at the point where the basal coil opens into the vestibule, and it tapers until it ends blindly at the apex. The otherwise hollow centre of the modiolus contains the cochlear artery and vein, as well as the twisted trunk of fibres of the cochlear nerve. This nerve, a division of the very short vestibulocochlear nerve, enters the base of the modiolus from the brainstem through an opening in the petrous portion of the temporal bone called the internal meatus. The spiral ganglion cells of the cochlear nerve are found in a bony spiral canal winding around the central core.
A thin bony shelf, the osseous spiral lamina, winds around the modiolus like the thread of a screw. It projects about halfway across the cochlear canal, partly dividing it into two compartments, an upper chamber called the scala vestibuli(vestibular ramp) and a lower chamber called the scala tympani (tympanic ramp). The scala vestibuli and scala tympani, which are filled with perilymph, communicate with each other through an opening at the apex of the cochlea, called the helicotrema, which can be seen if the cochlea is sliced longitudinally down the middle. At its basal end, near the middle ear, the scala vestibuli opens into the vestibule. The basal end of the scala tympani ends blindly just below the round window. Nearby is the opening of the narrow cochlear aqueduct, through which passes the perilymphatic duct. This duct connects the interior of the cochlea with the subdural space in the posterior cranial fossa (the rear portion of the floor of the cranial cavity).
A smaller scala, called the cochlear duct (scala media), lies between the larger vestibular and tympanic scalae; it is the cochlear portion of the membranous labyrinth. Filled with endolymph, the cochlear duct ends blindly at both ends—i.e., below the round window and at the apex. In cross sectionthis duct resembles a right triangle. Its base is formed by the osseous spiral lamina and the basilar membrane, which separate the cochlear duct from the scala tympani. Resting on the basilar membrane is the organ of Corti, which contains the hair cells that give rise to nerve signals in response to sound vibrations. The side of the triangle is formed by two tissues that line the bony wall of the cochlea: the stria vascularis, which lines the outer wall of the cochlear duct, and the fibrous spiral ligament, which lies between the stria and the bony wall of the cochlea. A layer of flat cells bounds the stria, separating it from the spiral ligament. The hypotenuse is formed by the transparent vestibular membrane (or Reissner membrane), which consists of only two layers of flattened cells. A low ridge, the spiral limbus, rests on the margin of the osseous spiral lamina. The Reissner membrane stretches from the inner margin of the limbus to the upper border of the stria.
The spiral ligament extends above the attachment of the Reissner membrane and is in contact with the perilymph in the scala vestibuli. Extending below the insertion of the basilar membrane, it is in contact with the perilymph of the scala tympani. It contains many stout fibres that anchor the basilar membrane and numerous connective-tissue cells. The structure of the spiral ligament is denser behind the stria than near the upper and lower margins. The spiral ligament, like the adjacent stria, is well supplied with blood vessels. It receives the radiating arterioles that pass outward from the modiolus in bony channels of the roof of the scala vestibuli. Branches from these vessels form a network of capillaries above the junction with the Reissner membrane that may be largely responsible for the formation of the perilymph from the blood plasma. Other branches enter the stria, and still others pass behind it to the spiral prominence. From these separate capillary networks, which are not interconnected, small veins descending below the attachment of the basilar membrane collect blood and deliver it to the spiral vein in the floor of the scala tympani.
At the lower margin of the stria is the spiral prominence, a low ridge parallel to the basilar membrane that contains its own set of longitudinally directed capillary vessels. Below the prominence is the outer sulcus. The floor of the outer sulcus is lined by cells of epithelial origin, some of which send long projections into the substance of the spiral ligament. Between these so-called root cells, capillary vessels descend from the spiral ligament. This region appears to have an absorptive rather than a secretory function, and it may be involved in removing waste materials from the endolymph.
In humans the basilar membrane is about 30 to 35 mm in length. It widens from less than 0.1 mm near its basal end to 0.5 mm near the apex. The basilar membrane is spanned by stiff elastic fibres that are connected at their basal ends in the modiolus. Their distal ends are embedded in the membrane but are not actually attached, which allows them to vibrate. The fibres decrease in calibre and increase in length from the basal end of the cochlea near the middle ear to the apex, so that the basilar membrane as a whole decreases remarkably in stiffness from base to apex. Furthermore, at the basal end the osseous spiral lamina is broader, the stria vascularis wider, and the spiral ligament stouter than at the apex. In contrast, however, the mass of the organ of Corti is least at the base and greatest at the apex. Thus, a certain degree of tuning is provided in the structure of the cochlear duct and its contents. With greater stiffness and less mass, the basal end is more attuned to the sounds of higher frequencies. Decreased stiffness and increased mass render the apical end more responsive to lower frequencies.
Beneath the fibrillar layer of the basilar membrane is the acellular ground substance of the membrane. This layer is covered in turn by a single layer of spindle-shaped mesothelial cells, which have long processes arranged longitudinally and parallel, facing the scala tympani and forming the tympanic lamella that is in contact with the perilymph.
Capillary blood vessels are found on the underside of the tympanic lip of the limbus and, in some species, including the guinea pig and humans, within the basilar membrane, beneath the tunnel. These vessels, called spiral vessels, do not enter the organ of Corti but are thought to supply most of the oxygen and other nutrients to its cells. Although the outer spiral vessel is seldom found in adult animals of certain species such as the dog, cat, and rat and is not found in the basilar membrane of every adult human, it is present in the human fetus. Its impressive diameter in the fetus suggests that it is an important channel for blood delivery to the developing organ of Corti.
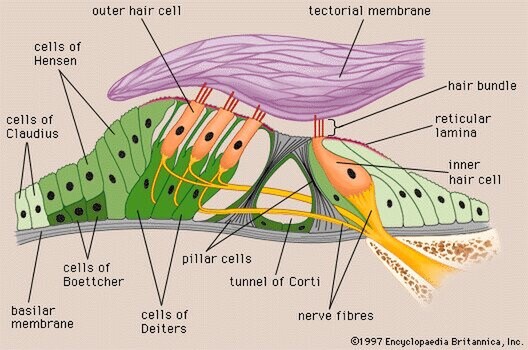
Organ of Corti
Arranged on the surface of the basilar membrane are orderly rows of the sensory hair cells, which generate nerve impulses in response to sound vibrations. Together with their supporting cells they form a complex neuroepithelium called the basilar papilla, or organ of Corti. The organ of Corti is named after Italian anatomist Alfonso Corti, who first described it in 1851.
Viewed in cross section, the most striking feature of the organ of Corti is the arch, or tunnel, of Corti, formed by two rows of pillar cells, or rods. The pillar cells furnish the major support of this structure. They separate a single row of larger, pear-shaped inner hair cellsfrom three or more rows of smaller, cylindrical outer hair cells. The inner hair cells are supported and enclosed by the inner phalangeal cells, which rest on the thin outer portion, called the tympanic lip, of the spiral limbus. On the inner side of the inner hair cells and the cells that support them is a curved furrow called the inner sulcus. This is lined with more or less undifferentiated cuboidal cells.
Each outer hair cell is supported by a phalangeal cell of Deiters, or supporting cell, which holds the base of the hair cell in a cup-shaped depression. From each Deiters’ cell a projection extends upward to the stiff membrane, the reticular lamina, that covers the organ of Corti. The top of the hair cell is firmly held by the lamina, but the body is suspended in fluid that fills the space of Nuel and the tunnel of Corti. Although this fluid is sometimes referred to as cortilymph, its composition is thought to be similar, if not identical, to that of the perilymph. Beyond the hair cells and the Deiters’ cells are three other types of epithelial cells, usually called the cells of Hensen, Claudius, and Boettcher, after the 19th-century anatomists who first described them. Their function has not been established, but they are assumed to help in maintaining the composition of the endolymph by ion transport and absorptive activity.
Each hair cell has a cytoskeleton composed of filaments of the protein actin, which imparts stiffness to structures in which it is found. The hair cell is capped by a dense cuticular plate, composed of actin filaments, which bears a tuft of stiffly erect stereocilia, also containing actin, of graded lengths arranged in a staircase pattern. This so-called hair bundle has rootlets anchored firmly in the cuticular plate. On the top of the inner hair cells 40 to 60 stereocilia are arranged in two or more irregularly parallel rows. On the outer hair cells approximately 100 stereocilia form a W pattern. At the notch of the W the plate is incomplete, with only a thin cell membrane taking its place. Beneath the membrane is the basal body of a kinocilium, although no motile ciliary (hairlike) portion is present as is the case on the hair cells of the vestibular system.
The stereocilia are about 3 to 5 μm in length. The longest make contact with but do not penetrate the tectorial membrane. This membrane is an acellular gelatinous structure that covers the top of the spiral limbus as a thin fibrillar layer, then becomes thicker as it extends outward over the inner sulcus and the reticular lamina. Its fibrils extend radially and somewhat obliquely to end at its lateral border, just above the junction of the reticular lamina and the cells of Hensen. In the upper turns of the cochlea, the margin of the membrane ends in fingerlike projections that make contact with the stereocilia of the outermost hair cells.
The myelin-ensheathed fibres of the vestibulocochlear nervefan out in spiral fashion from the modiolus to pass into the channel near the root of the osseous spiral lamina, called the canal of Rosenthal. The bipolar cell bodies of these neuronsconstitute the spiral ganglion. Beyond the ganglion their distal processes extend radially outward in the bony lamina beneath the limbus to pass through an array of small pores directly under the inner hair cells, called the habenula perforata. Here the fibres abruptly lose their multilayered coats of myelin and continue as thin, naked, unmyelinated fibres into the organ of Corti. Some fibres form a longitudinally directed bundle running beneath the inner hair cells and another bundle just inside the tunnel, above the feet of the inner pillar cells. The majority of the fibres (some 95 percent in the human ear) end on the inner hair cells. The remainder cross the tunnel to form longitudinal bundles beneath the rows of the outer hair cells on which they eventually terminate.
The endings of the nerve fibres beneath the hair cells are of two distinct types. The larger and more numerous endings contain many minute vesicles, or liquid-filled sacs, containing neurotransmitters, which mediate impulse transmission at neural junctions. These endings belong to a special bundle of nerve fibres that arise in the brainstem and constitute an efferent system, or feedback loop, to the cochlea. The smaller and less numerous endings contain few vesicles or other cell structures. They are the terminations of the afferent fibres of the cochlear nerve, which transmit impulses from the hair cells to the brainstem (see The physiology of hearing: Cochlear nerve and central auditory pathways).
The total number of outer hair cells in the cochlea has been estimated at 12,000 and the number of inner hair cells at 3,500. Although there are about 30,000 fibres in the cochlear nerve, there is considerable overlap in the innervation of the outer hair cells. A single fibre may supply endings to many hair cells, which thus share a “party line.” Furthermore, a single hair cell may receive nerve endings from many fibres. The actual distribution of nerve fibres in the organ of Corti has not been worked out in detail, but it is known that the inner hair cells receive the majority of afferent fibre endings without the overlapping and sharing of fibres that are characteristic of the outer hair cells.
Viewed from above, the organ of Corti with its covering, the reticular lamina, forms a well-defined mosaic pattern. In humans the arrangement of the outer hair cells in the basal turn of the cochlea is quite regular, with three distinct and orderly rows; but in the higher turns of the cochlea the arrangement becomes slightly irregular, as scattered cells form fourth or fifth rows. The spaces between the outer hair cells are filled by oddly shaped extensions (phalangeal plates) of the supporting cells. The double row of head plates of the inner and outer pillar cells cover the tunnel and separate the inner from the outer hair cells. The reticular lamina extends from the inner border cells near the inner sulcus to the Hensen cells but does not include either of these cell groups. When a hair cell degenerates and disappears as a result of aging, disease, or noise-induced injury, its place is quickly covered by the adjacent phalangeal plates, which expand to form an easily recognized “scar.”
Endolymph and perilymph
The perilymph, which fills the space within the bony labyrinth surrounding the membranous labyrinth, is similar, but not identical, in composition to other extracellular fluids of the body, such as cerebrospinal fluid. The concentration of sodium ions in the perilymph is high (about 150 milliequivalents per litre), and that of potassium ions is low (about 5 milliequivalents per litre), as is true of other extracellular fluids. Like these fluids, the perilymph is apparently formed locally from the blood plasma by transport mechanisms that selectively allow substances to cross the walls of the capillaries. Although it is anatomically possible for cerebrospinal fluid to enter the cochlea by way of the perilymphatic duct, experimental studies have made it appear unlikely that the cerebrospinal fluid is involved in the normal production of perilymph.
The membranous labyrinth is filled with endolymph, which is unique among extracellular fluids of the body, including the perilymph, in that its potassium ion concentration is higher (about 140 milliequivalents per litre) than its sodium ion concentration (about 15 milliequivalents per litre).
The process of formation of the endolymph and the maintenance of the difference in ionic composition between it and perilymph are not yet completely understood. The Reissner membrane forms a selective barrier between the two fluids. Blood-endolymph and blood-perilymph barriers, which control the passage of substances such as drugs from the blood to the inner ear, appear to exist as well. Evidence indicates that the endolymph is produced from perilymph as a result of selective ion transport through the epithelial cells of the Reissner membrane and not directly from the blood. The secretory tissue called the stria vascularis, in the lateral wall of the cochlear duct, is thought to play an important role in maintaining the high ratio of potassium ions to sodium ions in the endolymph.
Other tissues of the cochlea, as well as the dark cells of the vestibular organs, which must produce their own endolymph, are also thought to be involved in maintaining the ionic composition of the endolymph. Because the membranous labyrinth is a closed system, the questions of flow and removal of the endolymph are also important. The endolymph is thought to be reabsorbed from the endolymphatic sac, although this appears to be only part of the story. Other cochlear and vestibular tissues may also have important roles in regulating the volume and maintaining the composition of the inner-ear fluids.
The physiology of hearing
Hearing is the process by which the ear transforms soundvibrations in the external environment into nerve impulses that are conveyed to the brain, where they are interpreted as sounds. Sounds are produced when vibrating objects, such as the plucked string of a guitar, produce pressure pulses of vibrating air molecules, better known as sound waves. The ear can distinguish different subjective aspects of a sound, such as its loudness and pitch, by detecting and analyzing different physical characteristics of the waves. Pitch is the perception of the frequency of sound waves—i.e., the number of wavelengths that pass a fixed point in a unit of time. Frequency is usually measured in cycles per second, or hertz. The human ear is most sensitive to and most easily detects frequencies of 1,000 to 4,000 hertz, but at least for normal young ears the entire audible range of sounds extends from about 20 to 20,000 hertz. Sound waves of still higher frequency are referred to as ultrasonic, although they can be heard by other mammals. Loudness is the perception of the intensity of sound—i.e., the pressure exerted by sound waves on the tympanic membrane. The greater their amplitude or strength, the greater the pressure or intensity, and consequently the loudness, of the sound. The intensity of sound is measured and reported in decibels (dB), a unit that expresses the relative magnitude of a sound on a logarithmic scale. Stated in another way, the decibel is a unit for comparing the intensity of any given sound with a standard sound that is just perceptible to the normal human ear at a frequency in the range to which the ear is most sensitive. On the decibel scale, the range of human hearing extends from 0 dB, which represents a level that is all but inaudible, to about 130 dB, the level at which sound becomes painful.
In order for a sound to be transmitted to the central nervous system, the energy of the sound undergoes three transformations. First, the air vibrations are converted to vibrations of the tympanic membrane and ossicles of the middle ear. These in turn become vibrations in the fluid within the cochlea. Finally, the fluid vibrations set up traveling waves along the basilar membrane that stimulate the hair cells of the organ of Corti. These cells convert the sound vibrations to nerve impulses in the fibres of the cochlear nerve, which transmits them to the brainstem, from which they are relayed, after extensive processing, to the primary auditory area of the cerebral cortex, the ultimate centre of the brain for hearing. Only when the nerve impulses reach this area does the listener become aware of the sound.
Humans - We are amazing!
So now we have a good understanding of the human ear anatomy, next time we will talk about the importance of how the mechanics of our ears effects us as SCUBA divers - Equalisation.